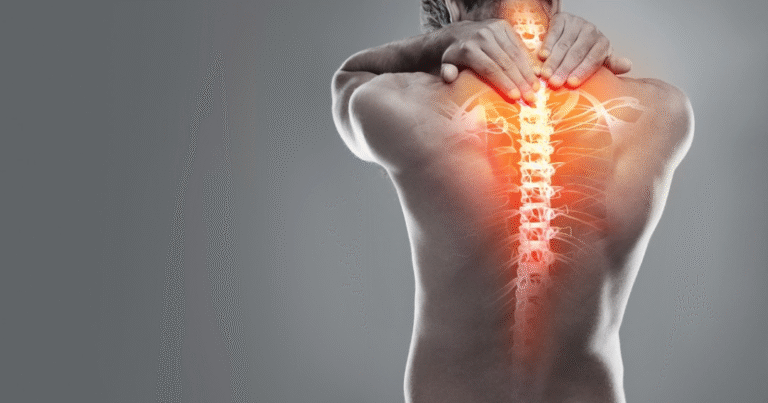
Chronic pain disorders are some of the most misunderstood and underdiagnosed conditions in modern medicine. While diseases like arthritis, fibromyalgia, and chronic fatigue syndrome are increasingly recognized, there remain many poorly defined pain syndromes that still challenge patients and healthcare providers alike. One such conceptual term is Inomyalgia—a word that, while not officially recognized in medical literature, evokes the complex reality of persistent muscle pain rooted in multiple biological and psychological factors.
What Is Inomyalgia?
The term “Inomyalgia” can be broken down into two parts:
-
“Ino-”: from the Greek inos, meaning “muscle” or “fiber.”
-
“-myalgia”: medical suffix meaning “muscle pain.”
Together, Inomyalgia can be interpreted as “pain arising from muscles or connective tissue.”
Like fibromyalgia, Inomyalgia could describe a chronic pain syndrome that involves widespread or localized muscle discomfort, stiffness, and tenderness. Unlike acute muscle pain caused by injury, Inomyalgia would represent a long-term, systemic condition that affects both body and mind.
Symptoms of Inomyalgia
If defined as a condition, Inomyalgia might present with a wide variety of symptoms, often fluctuating in severity:
-
Chronic Muscle Pain
Persistent aching or throbbing pain in multiple muscle groups. -
Stiffness and Tension
Muscles may feel tight, especially after periods of rest. -
Fatigue
Constant tiredness that is not relieved by sleep. -
Tender Points
Specific areas of the body may be sensitive to touch or pressure. -
Sleep Disturbances
Difficulty falling asleep, frequent waking, or non-restorative sleep. -
Cognitive Fog
Trouble concentrating, memory lapses, or slowed thinking (“brain fog”). -
Mood Symptoms
Anxiety, irritability, or depression often associated with chronic discomfort.
The diversity of symptoms makes Inomyalgia a multifaceted condition, affecting both physical and emotional well-being.
Possible Causes and Risk Factors
The origins of Inomyalgia would likely be multifactorial, combining biological, environmental, and psychological triggers. Potential causes include:
-
Nervous System Dysregulation: Overactive pain signals in the central nervous system.
-
Mitochondrial Dysfunction: Reduced cellular energy production leading to muscle fatigue.
-
Stress and Trauma: Chronic stress or past trauma potentially exacerbating symptoms.
-
Hormonal Imbalances: Irregularities in serotonin, cortisol, or thyroid hormones.
-
Genetic Susceptibility: Family history of chronic pain or autoimmune conditions.
-
Lifestyle Factors: Poor sleep, sedentary habits, or overexertion worsening pain cycles.
While not tied to a single cause, Inomyalgia would likely develop as the result of interacting systems gone awry.
Challenges in Diagnosis
One of the biggest hurdles with conditions like Inomyalgia is diagnostic uncertainty. Because symptoms overlap with fibromyalgia, chronic fatigue syndrome, depression, and autoimmune diseases, patients might:
-
Face years of misdiagnosis.
-
Be told their pain is “psychological.”
-
Struggle to validate their experiences in medical settings.
If recognized, Inomyalgia would require a diagnosis of exclusion, meaning other conditions must first be ruled out. This highlights the need for more biomarkers and diagnostic tests to detect underlying mechanisms of chronic pain disorders.
Treatment Approaches
Managing Inomyalgia would require a holistic, multi-pronged approach since no single treatment could address all symptoms. Possible interventions might include:
1. Medications
-
Analgesics: Non-opioid pain relievers for daily discomfort.
-
Antidepressants: To regulate neurotransmitters linked to pain perception.
-
Anticonvulsants: Sometimes used to calm overactive nerve signals.
2. Physical Therapy
Gentle stretching, low-impact exercise, and massage to maintain mobility and reduce stiffness.
3. Cognitive-Behavioral Therapy (CBT)
Helping patients reframe pain perception and cope with the emotional toll.
4. Lifestyle Modifications
-
Improved Sleep Hygiene
-
Balanced Diet Rich in Anti-inflammatory Foods
-
Regular Mind-Body Practices (yoga, tai chi, meditation).
5. Alternative Therapies
Acupuncture, aromatherapy, and herbal supplements may provide relief for some individuals.
The key lies in personalized care plans tailored to each patient’s unique symptoms and triggers.
Impact on Quality of Life
Living with Inomyalgia would be more than a medical challenge—it would shape nearly every aspect of daily living:
-
Work: Chronic pain may reduce productivity and lead to missed days.
-
Relationships: Friends and family may not fully understand invisible pain.
-
Mental Health: Constant discomfort often leads to depression or anxiety.
-
Self-Identity: Patients may struggle with self-esteem or feelings of limitation.
Support networks, patient advocacy, and social awareness are crucial in improving the lives of those who experience conditions like Inomyalgia.
The Broader Significance
Even though Inomyalgia is a conceptual condition, discussing it has broader importance:
-
Raises Awareness: Highlights the struggles of people with chronic, misunderstood pain.
-
Encourages Research: Inspires further exploration into neuromuscular and pain syndromes.
-
Empowers Patients: Validates the experiences of those whose pain does not fit neatly into existing diagnoses.
-
Promotes Holistic Health: Underscores the need for integrated care that bridges medicine, psychology, and lifestyle.
Future Directions
If Inomyalgia were to be recognized in medical literature, future developments could include:
-
Biomarker Identification: Pinpointing measurable indicators in blood, genetics, or brain scans.
-
Advanced Pain Therapies: Novel treatments using neuromodulation or regenerative medicine.
-
AI-Based Diagnostics: Using big data to detect patterns across patient populations.
-
Public Health Awareness: Campaigns to reduce stigma and promote early intervention.
With these advancements, Inomyalgia could shift from a poorly understood syndrome to a well-managed condition supported by medical science and social acceptance.
Conclusion
Inomyalgia, while not an officially recognized disorder, symbolizes the complex reality of chronic pain that millions of people face worldwide. By framing it as a syndrome of persistent muscle pain, fatigue, and cognitive challenges, we can better understand the struggles of individuals whose conditions remain invisible or misunderstood.
Though challenges in diagnosis, treatment, and awareness persist, the exploration of Inomyalgia highlights a crucial truth: chronic pain deserves recognition, compassion, and innovation in care.